The anterior cruciate ligament [ACL] plays a vital role in the stability of the knee joint, preventing anterior translation of the tibia on the femur as well as providing rotational stability and preventing excessive hyperextension (Levangie & Norkin, 2011). Movements such as rapid deceleration, hyperextension or sudden rotation place an increased load on the ACL and can result in rupture (Dai et al., 2019). Rupture of the ACL is a highly prevalent musculoskeletal injury in Australia (Lobb, Tumilty & Claydon, 2012). Once ruptured, the surrounding tissue damage and lack of stability have been known to contribute to secondary knee pathologies, such as osteoarthritis and meniscal damage (Ajuied et al., 2013).
Present day knowledge dictates that athletes wanting to return to sport, younger individuals, and patients who experience knee instability despite rehabilitation are likely candidates for ACL reconstruction surgery (Dhillon, 2014). Arthroscopically assisted ACLR using either the patella or hamstring tendon is the standard surgical treatment for patients (Gianotti, Marshall, Hume & Bunt, 2009). Magnussen, Carey and Spindler (2010) found in their systematic review that there is no significant difference in knee stability and strength between those two grafts.
There is general consensus that physiotherapy plays an important role in the rehabilitation of ACL reconstruction patients to premorbid level of function post-operatively. The rehabilitation progresses essential components of a knee’s function, such as range of motion, stability, neuromuscular control and arguably the most significant: quadriceps’ strength (Cooper & Hughes, 2017). Grindem, Snyder-Mackler, Moksnes, Engebretsen and Risberg (2016) found a 33 per cent re‑injury rate in patients that had less than 90 per cent strength of their non ACLR leg. The challenge during the early stages of rehabilitation is that the graft is undergoing increasing necrosis and hypocellularity, markedly at the centre of the graft, resulting in reduced graft mechanical strength (Janssen & Scheffler, 2013). Despite this, it is vital that this graft and tissue are mechanically loaded, however the level of load is paramount. If the graft is under‑loaded it can lead to significant loss of tensile strength (Ménétrey, Duthon, Laumonier & Fritschy, 2008), whereas conversely, a significant overload of mechanical stress can similarly reduce graft tensile strength (Ekdahl, Wang, Ronga & Fu, 2008).
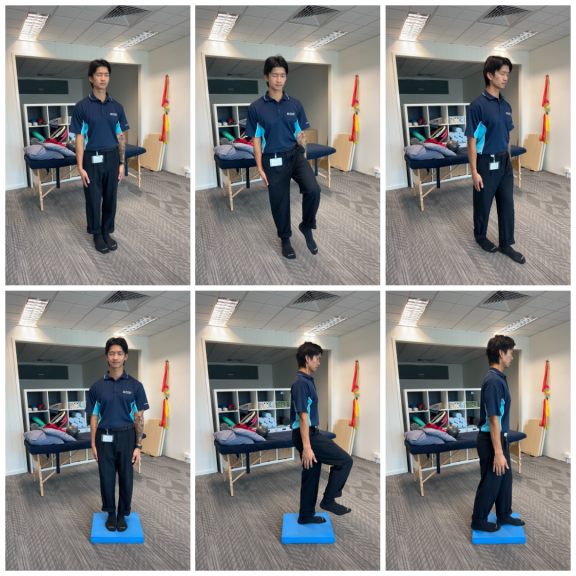
It is recognised that overloading the graft contributes to graft laxity (Cuomo, Reddi Boddu Siva Rama, Bull & Amis, 2007). ACL graft laxity risks compromising normal knee biomechanics through increased tibial anterior translation and internal rotation, resulting in increased contact stress (Simon et al., 2015). Therefore, ACL graft laxity can significantly contribute to secondary meniscal degeneration, subchondral sclerosis (Kiapour & Murray, 2014) and graft re-rupture (Hewett, 2017). For this reason the open kinetic chain [OKC] versus closed kinetic chain [CKC] approach is heavily debated. It is speculated that OKC exercises (where the distal segment of the limb is free to move) result in increased anterior tibial translation and hence overload the new graft (Escamilla, Macleod, Wilk, Paulos & Andrews, 2012). The use of CKC exercises conversely, (where the distal segment of the limb is fixated) is encouraged in the ACLR rehabilitation process and can be dated back to recommendations made by Henning, Lynch and Glick (1985). It is hypothesised that CKC reduces tibial anterior displacement secondary to co‑contraction of the hamstrings in combination with joint compression forces (Escamilla et al., 2012). CKC exercise is not always practical however. Sigward, Chan, Lin, Almansouri and Pratt (2018) found that an ACLR patient will compensate away from their reconstructed knee through weight distribution for at least 5 months post-operatively during loaded or unloaded squats. This weight distribution coupled with the body’s ability to compensate for weak quadriceps by engaging gluteus maximus and calf muscles to achieve knee extension (Thompson, Chaudhari, Schmitt, Best & Siston, 2013) means that quadriceps’ strength adaptations can be difficult to achieve in CKC. Furthermore Escamilla et al. (2012) showed that a 12-repetition maximum knee extension from 0-90 degrees has comparable, if not less, peak shear forces on the ACL than walking across level ground.
So, to OKC or to not OKC?
There is a moderate level of evidence to suggest that OKC exercises do not contribute to increased ACL laxity or reduced self-reported function during rehabilitation of ACLR when compared to CKC exercises. There is a significant need for a greater volume of high-quality research to help pilot new guidelines for practitioners of the multidisciplinary team. Until there is strong evidence, practitioners are advised to use clinical judgment and post operative orders as well as take a cautious approach when prescribing OKC exercises during the first 12 weeks of ACLR recovery. Should OKC exercises be prescribed, current evidence suggests they not be used as a replacement to CKC exercises but rather a supplement, and only when the exercise could not be substituted for a CKC exercise.References:
- Ajuied, A., Wong, F., Smith, C., Norris, M., Earnshaw, P., Back, D., & Davies, A. (2013). Anterior Cruciate Ligament Injury and Radiologic Progression of Knee Osteoarthritis. The American Journal of Sports Medicine, 42(9), 2242-2252. doi: 10.1177/0363546513508376
- Cooper, R., & Hughes, M. (2017). Melbourne ACL Rehabilitation Guide 2.0. Melbourne: Premax.
- Cuomo, P., Reddi Boddu Siva Rama, K., Bull, A., & Amis, A. (2007). The Effects of Different Tensioning Strategies on Knee Laxity and Graft Tension after Double-Bundle Anterior Cruciate Ligament Reconstruction. The American Journal of Sports Medicine, 35(12), 2083-2090. doi: 10.1177/0363546507308548
- Dai, B., Garrett, W., Gross, M., Padua, D., Queen, R., & Yu, B. (2019). The effect of performance demands on lower extremity biomechanics during landing and cutting tasks. Journal of Sport and Health Science, 8(3), 228-234. doi: 10.1016/j.jshs.2016.11.004
- Ekdahl, M., Wang, J., Ronga, M., & Fu, F. (2008). Graft healing in anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy, 16(10), 935-947. doi: 10.1007/s00167-008-0584-0
- Escamilla, R., Macleod, T., Wilk, K., Paulos, L., & Andrews, J. (2012). ACL Strain and Tensile Forces for Weight Bearing and Non—Weight-Bearing Exercises After ACL Reconstruction: A Guide to Exercise Selection. Journal of Orthopaedic & Sports Physical Therapy, 42(3), 208-220. doi: 10.2519/jospt.2012.3768
- Gianotti, S., Marshall, S., Hume, P., & Bunt, L. (2009). Incidence of anterior cruciate ligament injury and other knee ligament injuries: A national population-based study. Journal of Science and Medicine In Sport, 12(6), 622-627. doi: 10.1016/j.jsams.2008.07.005
- Grindem, H., Snyder-Mackler, L., Moksnes, H., Engebretsen, L., & Risberg, M. (2016). Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. British Journal of Sports Medicine, 50(13), 804-808. doi: 10.1136/bjsports-2016-096031
- Henning, C., Lynch, M., & Glick, K. (1985). An in vivo strain gage study of elongation of the anterior cruciate ligament. The American Journal of Sports Medicine, 13(1), 22-26. doi: 10.1177/036354658501300104
- Hewett, T. (2017). Editorial Commentary: Increased Risk of Second Ruptures and Poorer Outcomes After Anterior Cruciate Ligament Injury and Reconstruction in Hypermobile Athletes: A Potential Synergism of Passive Ligamentous and Active Muscular Control of Dynamic Knee Stability Related to Age and Sex?. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 33(10), 1859-1861. doi: 10.1016/j.arthro.2017.07.012
- Janssen, R., & Scheffler, S. (2013). Intra-articular remodelling of hamstring tendon grafts after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy, 22(9), 2102-2108. doi: 10.1007/s00167-013-2634-5
- Kiapour, A., & Murray, M. (2014). Basic science of anterior cruciate ligament injury and repair. Bone & Joint Research, 3(2), 20-31. doi: 10.1302/2046-3758.32.2000241
- Levangie, P., & Norkin, C. (2011). Joint Structure and Function (5th ed., pp. 405-408). Philadelphia: F.A. Davis Company.
- Lobb, R., Tumilty, S., & Claydon, L. (2012). A review of systematic reviews on anterior cruciate ligament reconstruction rehabilitation. Physical Therapy in Sport, 13(4), 270-278. doi: 10.1016/j.ptsp.2012.05.001
- Magnussen, R., Carey, J., & Spindler, K. (2010). Does autograft choice determine intermediate-term outcome of ACL reconstruction?. Knee Surgery, Sports Traumatology, Arthroscopy, 19(3), 462-472. doi: 10.1007/s00167-010-1277-z
- Ménétrey, J., Duthon, V., Laumonier, T., & Fritschy, D. (2008). “Biological failure” of the anterior cruciate ligament graft. Knee Surgery, Sports Traumatology, Arthroscopy, 16(3), 224-231. doi: 10.1007/s00167-007-0474-x
- Sigward, S., Chan, M., Lin, P., Almansouri, S., & Pratt, K. (2018). Compensatory Strategies That Reduce Knee Extensor Demand During a Bilateral Squat Change From 3 to 5 Months Following Anterior Cruciate Ligament Reconstruction. Journal of Orthopaedic & Sports Physical Therapy, 48(9), 713-718. doi: 10.2519/jospt.2018.7977
- Thompson, J., Chaudhari, A., Schmitt, L., Best, T., & Siston, R. (2013). Gluteus maximus and soleus compensate for simulated quadriceps atrophy and activation failure during walking. Journal of Biomechanics, 46(13), 2165-2172. doi: 10.1016/j.jbiomech.2013.06.033