During pregnancy, your body goes through a lot of changes to help grow and deliver the baby. While many of these changes are temporary, they may cause pain or limit how well you can move. The good news is, physiotherapists are well trained to help reduce pain and improve your movement. Here's some information on common problems during pregnancy and tips on how to manage them.

Many women experience lower back pain at some point during their pregnancy. This can happen because of:
Even though you might still have some back pain during your pregnancy, there are lots of ways physiotherapy can help reduce your pain and improve your movement and daily life.

Research shows that combining exercise with learning how to manage pain is very helpful in reducing back pain during pregnancy. It's important to talk to your physiotherapist about what exercises are safe for you. Some examples might include:
Your physiotherapist can also teach you pain management strategies, movement and activity modifications, positions of ease and physical activity recommendations.
Physiotherapists can also use hands-on techniques to help reduce your pain. These might include spinal mobilisations, muscle relaxation techniques, TENS (a machine that uses electrical impulses to reduce pain) or kinesio taping to help support your lower back.
There’s strong evidence to suggest that wearing special support garments can help with pregnancy-related lower back pain. Your physiotherapist can recommend what types of support wear might work best for you, such as tubigrip (a type of stretchy bandage), compression shorts/tights to support your belly and pelvic area as well as SIJ belts or belly bands for your lower back.
You may experience pain in certain areas of your pelvis during pregnancy and occasionally for a period after birth.
During pregnancy your body undergoes many changes to allow for your baby to grow. These may include:
PGP can present differently in different people. You may experience pain in your:
The carpal tunnel is a structural opening in the wrist which nerves and tendons pass from your arm into your hand and fingers. Increased fluid retention during pregnancy will often cause compression of the median nerve, leading to carpal tunnel syndrome.
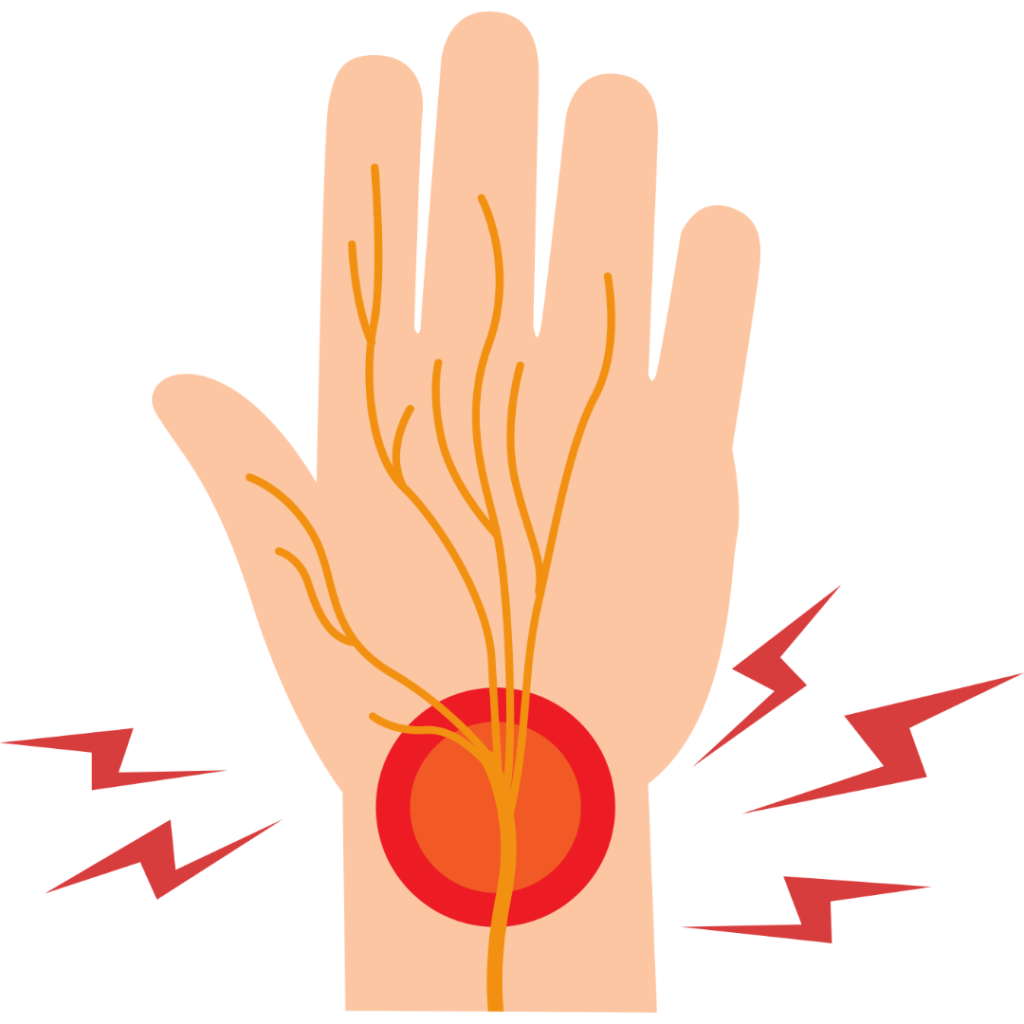
You may experience the following:
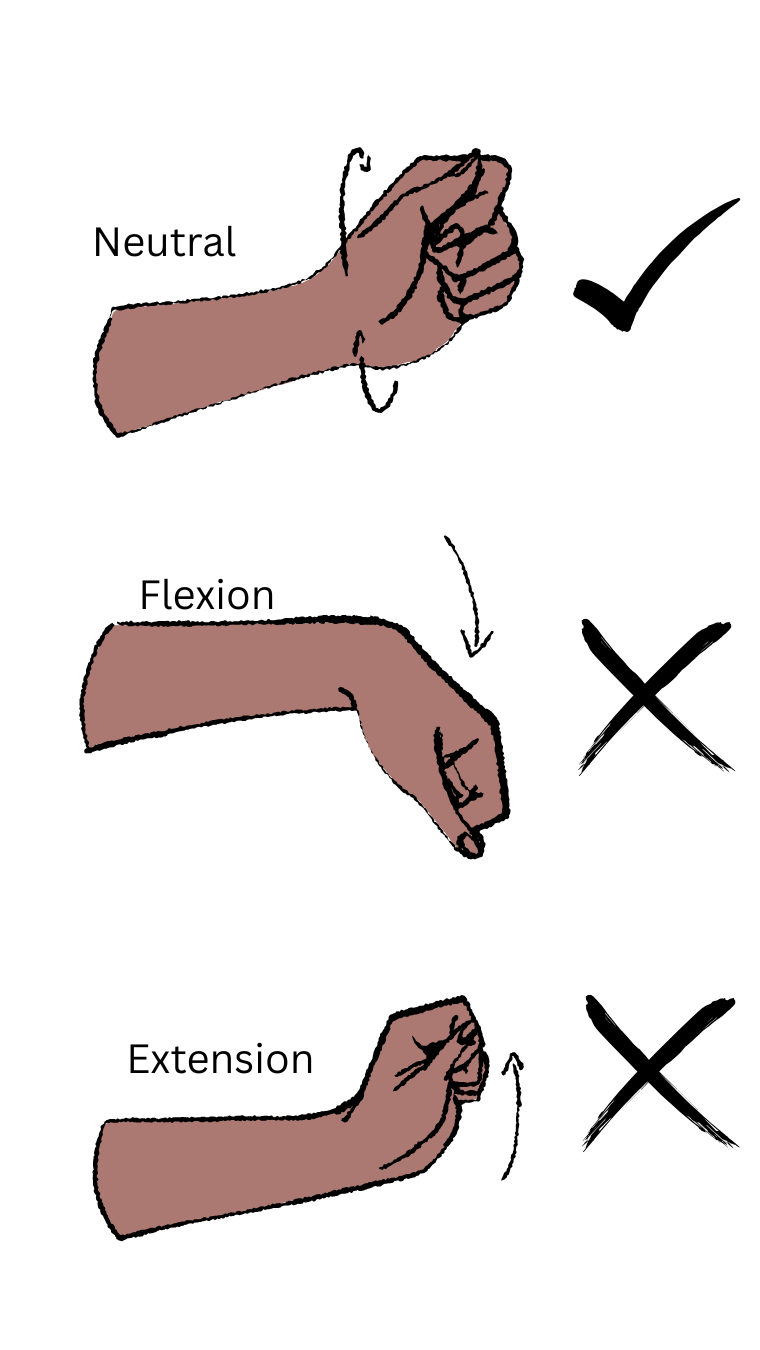
Often it can take at least 3-4 days after birth for the swelling in your body to start to reduce or show signs of improvement. While caring for your baby, it is important to try keep your wrist as neutral as possible. Especially when breastfeeding and or/carrying your baby to avoid aggravating your symptoms. You may continue to wear a wrist splint until your symptoms resolve. Use pillows for extra support while breastfeeding and discuss with your midwives’ alternate positions that feel right for you. If your symptoms show no signs of improvement with these strategies, it is important to seek guidance from a physiotherapist for the next steps in treating your carpal tunnel.
DRAM (also known as abdominal muscle separation) is the stretching of your connective tissue in your abdominal region as a result of your growing baby during pregnancy.
DRAM can occur due to multiple factors throughout your pregnancy (9). These may include:
There is evidence to suggest that low impact exercise (walking, cycling, Pilates) throughout pregnancy can reduce the severity of DRAM, though everyone will experience some degree of abdominal muscle separation likely in the third trimester.
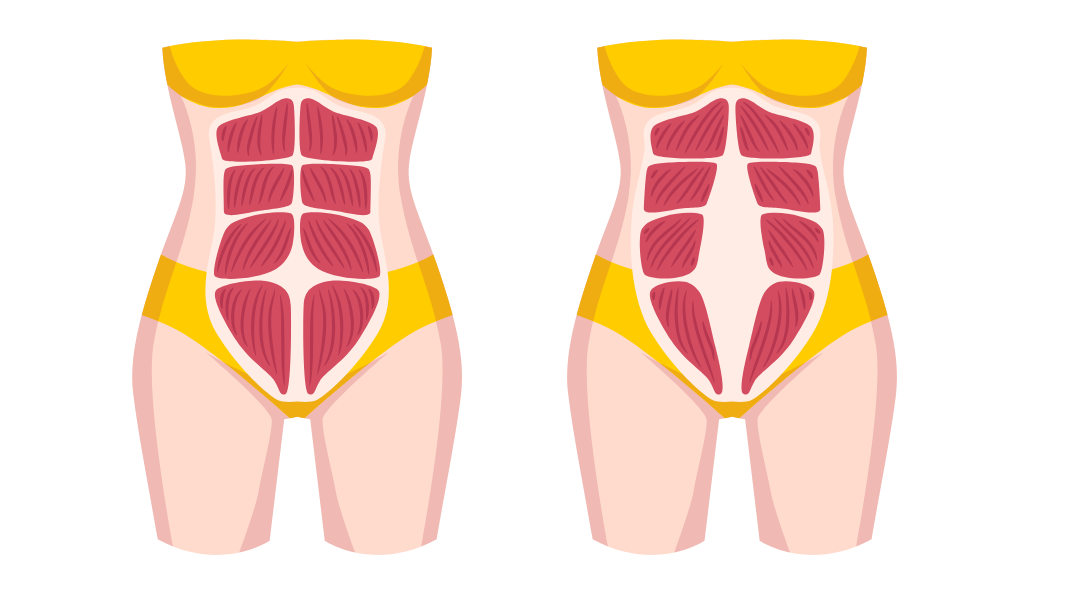
Our abdominal muscles are important as they provide support for our back and work together with our pelvic floor to support our pelvic organs after birth. While your abdominal wall can heal naturally in the months following birth, it is important to be mindful and continue to monitor it over time with your physiotherapist.
The pelvic floor is a group of muscles that work together to support your pelvic organs and help control your bladder and bowel. During pregnancy, these muscles can weaken due to the increased intra-abdominal pressure from the growing baby and other changes in the body. This can lead to the development of pelvic floor disorders, such as pelvic organ prolapse (POP), urinary incontinence (UI) and/or faecal incontinence (FI).
Research shows that training your pelvic floor muscles can help reduce or even stop problems like leaking urine and pelvic organ prolapse during pregnancy and after birth. Strengthening these muscles can make a big difference in both the amount and frequency of urine leakage, meaning you might not need long-term treatment. It is strongly recommended that pregnant women regularly do pelvic floor exercises with help from a health professional.