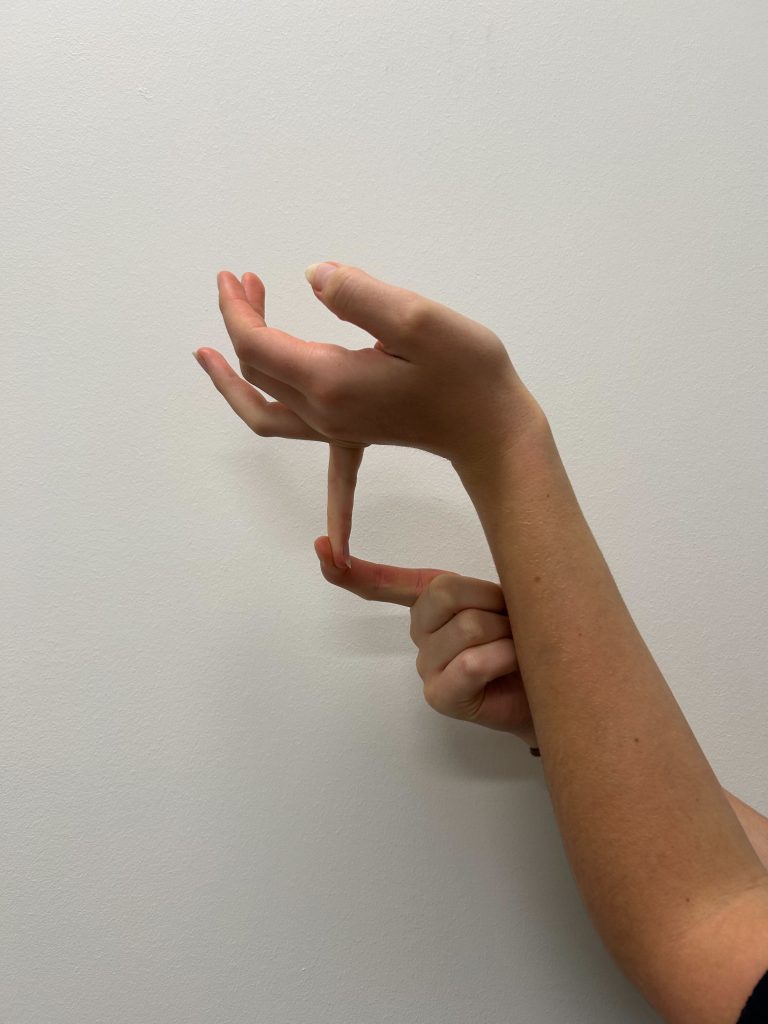
Joint hypermobility is a genetic condition characterised by overly flexible joints resulting in excessive range of movement. Joint hypermobility can be either localised (affecting one or a few joints) or generalised (affecting multiple joints across the body). It's most commonly assessed using the Beighton Score, a 9-point scale evaluating hypermobility in various joints. A score of 5 or more out of 9 suggests generalised joint hypermobility (GJH). It’s important to note that joint hypermobility can be completely benign in some people. However, in others, it is associated with pain, dysfunction, and additional health issues. In more complex cases, it may be diagnosed as part of a broader condition such as Hypermobility Spectrum Disorder (HSD) or Ehlers-Danlos Syndrome (EDS)—specifically the hypermobile type (hEDS).[1]
What are the Risk Factors?[1]
| Risk Factor | Why? |
| Age | Younger children tend to be more hypermobile. Ligaments tend to stiffen with age. |
| Sex | Hypermobility has a higher prevalence in women as compared to men. |
| Ethnicity | Certain populations, particularly Asian and African ethnicities, show higher prevalence due to genetic variation in connective tissue. |
| Genetics | A family history of hypermobility is a strong indicator, suggesting a genetic component in connective tissue makeup. |
What are the Clinical Features of Joint Hypermobility?[1]
- Joint instability, including prior history of partial dislocation (subluxation) and/or dislocations.
- Recurrent musculoskeletal pain.
- Soft, stretchy, or velvety skin, sometimes associated with certain subtypes of EDS

Joint Hypermobility is also Commonly Associated with: [1]
- Chronic fatigue.
- Easy bruising.
- Functional bowel disorders, think IBS for example.
- Cardiovascular conditions such as POTS (Postural Orthostatic Tachycardia Syndrome).
- Some neurological conditions.
- Immune disorders.
- Anxiety.
- Autism and ADHD.
- Bladder and pelvic floor dysfunction.[2]
What Effect Does Joint Hypermobility Have on Body Structure and Function?
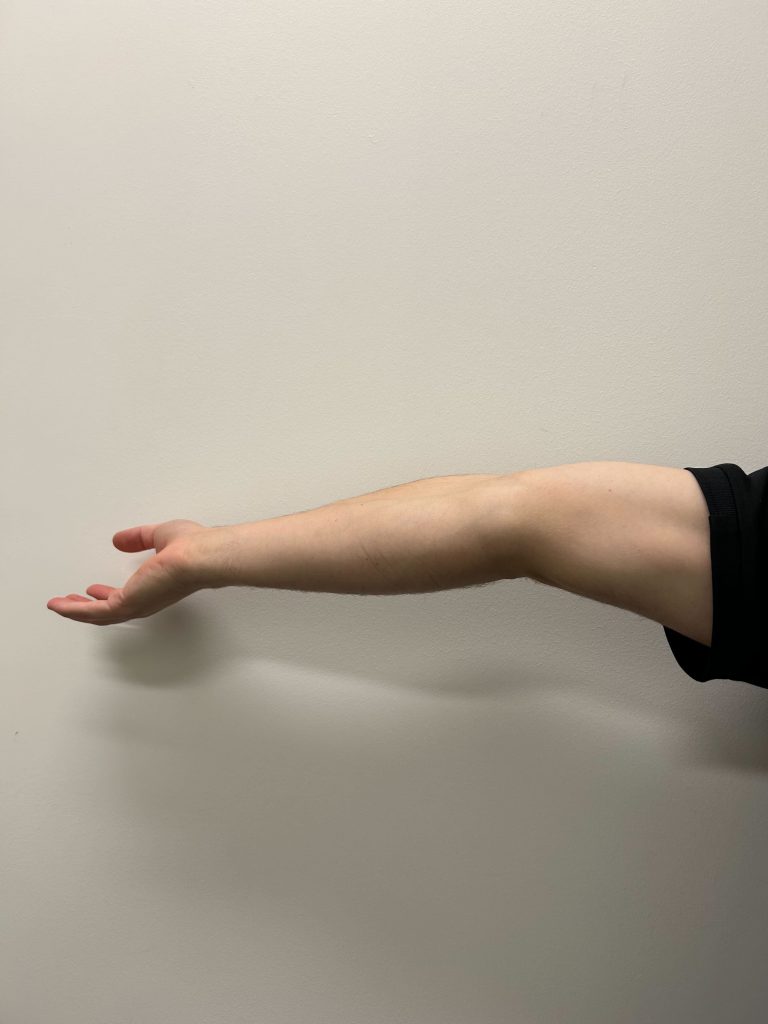
Certain types of connective tissue, like ligaments and tendons, help to provide stability to our joints; in the case of hypermobility, the connective tissue is extremely stretchy and flexible which means that there is less structural stability allowing your joints to go through a far greater range of motion. As a result, there is an increased risk of joint dislocation and subluxation (partial dislocation). Similarly, there is an increased risk of soft tissue injury, like a muscle or tendon strain, as the muscle fibres are being stretched beyond their limits.
Some studies have found that individuals with GJH have poorer joint position sense and threshold detection to movement, contributing to increased injury risk and impaired coordination.
Quality of Life: Beyond the Physical
Children and adolescents with GJH or hEDS often report feeling left out or frustrated because they cannot participate in physical activities like their peers. Many experience:
- Chronic pain
- Reduced physical function
- Fatigue
- Emotional distress
One study showed that pain intensity, symptom count, fatigue, and stress incontinence predicted quality of life, functional limitations, anxiety, and depression in youth with hypermobility.
Another study exploring children with fibromyalgia, GJH, and gastrointestinal symptoms found a high overlap of these conditions. Emotional distress may be a common thread linking these seemingly different symptoms.
What is the Management for Joint Hypermobility? Looking at the Science... [3]
Joint hypermobility is not something we can cure or fix through treatment; it requires ongoing self-management, particularly if you are participating in sports and specific types of physical activity. Research has shown that physiotherapy is effective in improving pain, strength and preventing injury for people with joint hypermobility. Physiotherapy may include:
- Progressive strength training; it is important for those with GJH to build and maintain strong muscles to help provide stability to your joints.
- Manual therapy; it is not uncommon to have tight muscles with GJH as the muscles are working extra hard to support the joints and prevent excessive movement.
- Motor control exercises; motor control refers to muscle memory and the orchestra of muscle movement. It is extremely important in GJH to have and maintain good motor control throughout the full joint range of motion, which often means training into hyperextension.
- Joint position sense re-training; also referred to as joint proprioception, is your knowledge about where your body or body part is in space. Poor proprioception can contribute to musculoskeletal pain or dysfunction as you can become unaware that you are sustaining poor postures ie. slouching or displaying a forward head posture.
- Education; research shows that having a good understanding of your condition, how it affects you and the best way to manage your symptoms can significantly improve patient outcomes, both mentally and physically.
What Type of Physical Activity is Recommended for People With Joint Hypermobility? [4]
Those with hypermobility may have been told they should avoid high impact sports like running or HIIT as well as contact sports because the risk of injury is high, and in some cases this may be an appropriate recommendation BUT with the right management, you can minimise your risk of injury and give yourself the best opportunity to continue doing what you love.
If you have joint hypermobility and are not sure where to start on your exercise journey, we recommend starting with low-impact exercise to build adequate strength and joint stability. Some common forms of low impact exercise include:
- Swimming: Great for cardiovascular fitness with minimal joint strain.
- Cycling: Builds leg strength and endurance.
- Pilates: Focuses on core control, alignment and strength.
- Yoga: When guided properly, can improve control and body awareness.
- Individualised exercise program: best developed with a physiotherapist or exercise physiologist.


When is it the Right Time to Seek Help?
You may consider seeking help from a physiotherapist for assistance managing your joint hypermobility if you:
- Are experiencing acute or persistent musculoskeletal pain.
- Have had one or multiple joint dislocations.
- Frequently get injured.
- Have been recently diagnosed with hypermobility and are unsure on how to manage.
Don't wait until symptoms escalate. Early intervention is key to preventing long-term dysfunction and maintaining an active, fulfilling life.
See our contact details below to book in your initial assessment with our experienced physiotherapists and take the first step towards managing your joint hypermobility today.oday.
Phone: 0395335305
Address: Unit 6/328 Reserve Road, Cheltenham, Victoria, 3192












