Osteoporosis is a condition that causes bones to become thin, brittle, and more likely to break. It’s often called the “silent disease” because it usually doesn’t show symptoms until a fracture occurs. A small fall, a bump into a wall, or even bending forward can result in a break if your bones are fragile.
But here’s the good news: the right kind of exercise can help improve bone strength, reduce the risk of falls, and maintain your independence as you age. In this article, we’ll explain:
- What osteoporosis is
- Why it happens
- How exercise can help
- Which types of exercise are most effective
- What the research says
- What to do if you already have fractures
- How to build an action plan for your bone health
What is Osteoporosis?
Osteoporosis means “porous bone.” It’s a condition where bones lose density and strength, becoming more likely to fracture under pressure. These fractures often happen in the hip, spine, or wrist. You may not even realise you have osteoporosis until you break a bone.
A DEXA scan is used to measure bone density. This scan gives you a T-score:
| Bone Density | Score |
| Normal Bone Density | T-score above -1 |
| Osteopenia (early bone loss) | Between -1 and -2.5 |
| Osteoporosis | Below -2.5 |
| Severe Osteoporosis | Below -2.5 with a fracture |
Osteoporosis is very common. Research estimates that around 137 million women and 21 million men are at high risk of osteoporotic fractures worldwide, and this number is expected to double in the next 40 years 1.
Why Do Bones Get Weaker?
Our bones are living tissues that rebuild themselves over time. But as we age, especially after menopause, bone breakdown starts to happen faster than bone building. This leads to bone thinning.
Several things increase your risk of developing osteoporosis, including:
- Ageing
- Menopause (due to decreased oestrogen)
- Family history of osteoporosis
- Smoking
- Excessive alcohol consumption
- Poor calcium or vitamin D intake
- Inactivity or long periods of sitting
- Certain medications like steroids
The result is reduced bone mass and a higher risk of fractures, especially from low-trauma events like falling from standing height.
Can Exercise Help?
Yes, absolutely. Exercise is one of the best ways to manage osteoporosis. It helps:
- Build or maintain bone density
- Improve balance and strength
- Reduce the risk of falls
- Improve posture and reduce spinal pain
- Support mental wellbeing and confidence
However, not all exercises are equally helpful. Some types are ideal for improving bone strength, while others are better for balance or posture. The key is to find the right type of exercise for your situation.
The “Strong, Steady and Straight” Framework
In 2021, a group of people living with osteoporosis, along with health professionals, developed a helpful way to understand what kinds of exercise are needed 2. They called it the “Strong, Steady and Straight” approach:
- Strong: Exercises that build bone and muscle strength, such as lifting weights or doing impact-based activities
- Steady: Exercises that improve balance and reduce falls risk, such as Tai Chi, Pilates, or standing balance drills
- Straight: Exercises that protect the spine, improve posture, and reduce the risk of spinal fractures
This approach came out of frustration from patients who had been told to avoid exercise entirely. But modern research shows that, when done safely, exercise is not only safe — it’s essential 2.
What the Research Tells US
1. Heavy Lifting Can Be Safe and Effective
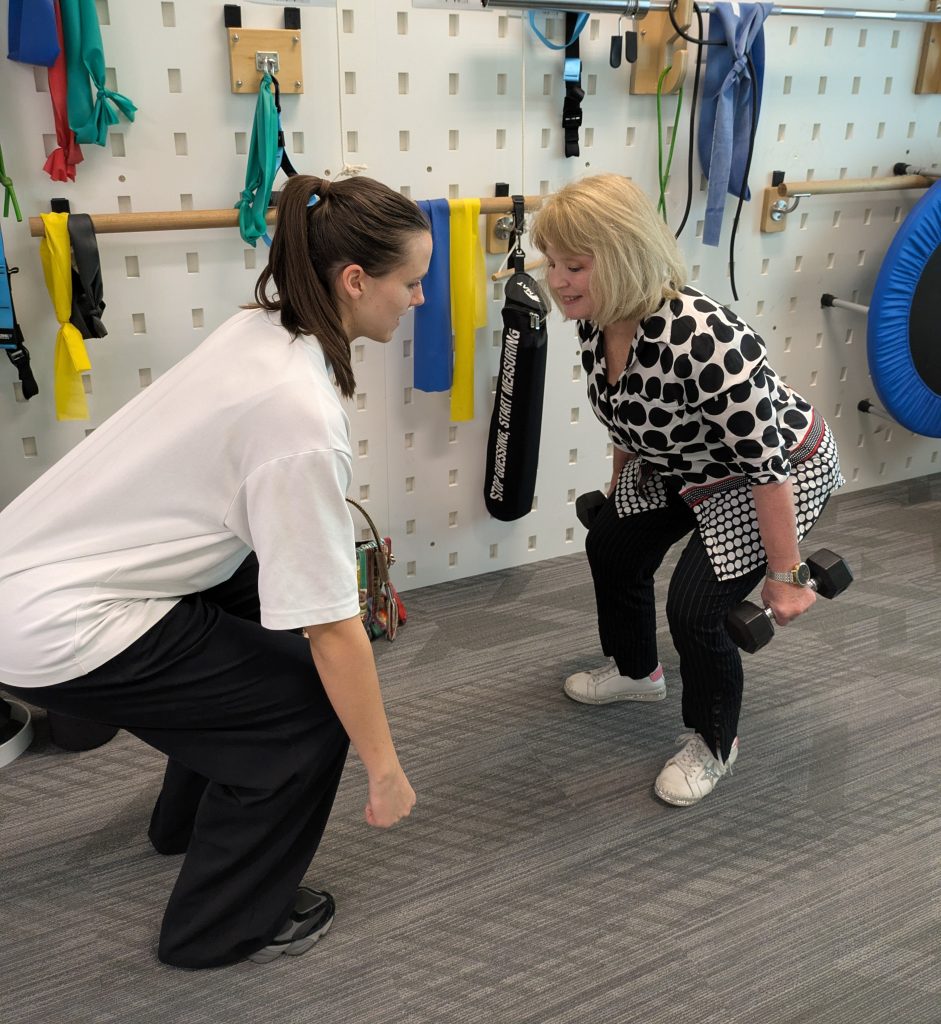
In the LIFTMOR trial, researchers studied women over the age of 58 with low bone density. Participants did a supervised strength training program two times per week for eight months. It included exercises like deadlifts, squats, and overhead presses, using 80 to 85 percent of their maximum strength.
Results showed improved bone density at the hip and spine — the areas most at risk of fracture 3.
This means that heavy lifting, done properly and under supervision, can help improve bone health even in older adults.
2. Jumping Improves Bone in Younger Adults
A meta-analysis by Zhao et al. (2014) found that jumping exercises helped increase bone density in the hip and thigh bones of premenopausal women 4. These exercises included jumping, hopping, and multidirectional movement.
Interestingly, jumping didn’t seem to improve bone density in the lower spine, which may need more targeted strengthening of spinal muscles.
For people who are younger or at lower risk of fracture, jumping exercises can be an excellent way to build strong bones.
3. Walking Isn't Enough on Its Own
Walking has many health benefits, including improved heart health and general fitness. But research shows that walking alone may not be strong enough to increase bone density — especially in the spine 5.
Walking may help maintain bone at the hip, particularly if done over a long period. But for real bone gains, you need higher-impact or resistance-based exercise.
What About Fall Prevention?
Most fractures happen because of a fall. So, reducing your chance of falling is just as important as improving your bone strength.
Research shows that regular balance and strength training significantly reduces the risk of falls in older people 6. These can include:
- Standing on one leg
- Heel-to-toe walking
- Sit-to-stand repetitions
- Balance exercises using cushions or foam pads
- Tai Chi or Pilates
Adding these into your weekly routine is essential for anyone over 65, especially those with existing bone loss.
How to Exercise with Spine Fractures
Many people with spinal fractures are unsure if they can exercise safely. The answer is yes — but with modifications.
If you’ve had a vertebral fracture or are at high risk:
| DO ✅ | DON'T ❌ |
| Focus on strengthening your spinal extensor muscles | Avoid deep forward bending, especially with weights |
| Use gentle, posture-based exercises like back extension or Pilates-style movements | Avoid twisting movements under load |
With the right guidance from a physiotherapist, you can still stay active and safe 2.
The Link Between Muscle Loss and Osteoporosis
As we age, we don’t just lose bone — we also lose muscle. This is called sarcopenia, and it’s strongly linked with osteoporosis. Muscle loss increases your risk of falling, breaking a bone, and losing independence.
Beaudart et al. (2016) found that sarcopenia affects up to 29 percent of older people living in the community, and up to 33 percent in aged care. It's also linked with lower quality of life, depression, and hospitalisation 7.
The good news? Sarcopenia can be prevented and reversed through:
- Resistance training 2 to 3 times per week
- Eating enough protein at each meal
- Staying generally active
You can check your risk of sarcopenia using tools like the SARC-F questionnaire or grip strength and walking tests.
What About Nutrition?
Nutrition plays a big role in bone and muscle health. While calcium and vitamin D are important, most people don't need high doses unless they're deficient.
Chen et al. (2019) suggest that the best results come from combining good nutrition with exercise and falls prevention 8.
Key nutrients include:
| Nutrient | Source in Diet |
| Calcium | Dairy, leafy greens, almonds |
| Vitamin D | Oily fish, supplements and the sun! |
| Protein | Meat, eggs, tofu, legumes |
Eating well supports the effect of exercise and helps your body build and maintain healthy bone and muscle.
Putting It All Together: Your Bone Health Action Plan
Here’s a simple plan to improve or protect your bone health:
- Get a DEXA scan if you’re over 50 or have risk factors
- Start a strength training program – ideally supervised by a physiotherapist
- Add balance and posture exercises to reduce fall risk
- Avoid spine-loading movements if you have fractures
- Eat a balanced diet with enough calcium, vitamin D, and protein
- Quit smoking and limit alcohol
- Stay active daily, even with low-impact movement like walking or Tai Chi
- Get professional advice to design a program that’s right for you
Final Thoughts
Osteoporosis does not mean you have to stop moving. In fact, safe and effective movement is one of the best ways to manage your condition and maintain your independence.
Whether you’re at risk of osteoporosis, already have low bone density, or have had a fracture, there’s always something you can do to improve your bone and muscle health.
At Peak MSK Physio, we help people of all ages stay strong, steady, and straight with evidence-based, personalised physiotherapy programs.
Need help getting started?
Book a bone health consultation with us in the clinic.
Let’s build stronger bones together.












