Knee injuries are some of the most common injuries within the population. They can affect younger people through Osgood-Schlatter disease. They can impact active people in their 20’s and 30’s, who can suffer from an ACL injury. Of course, those in the older demographic are susceptible to more chronic injuries like Osteoarthritis. As you can see, whether you are young, old or somewhere in between, it’s important you understand how to take care of your knees.
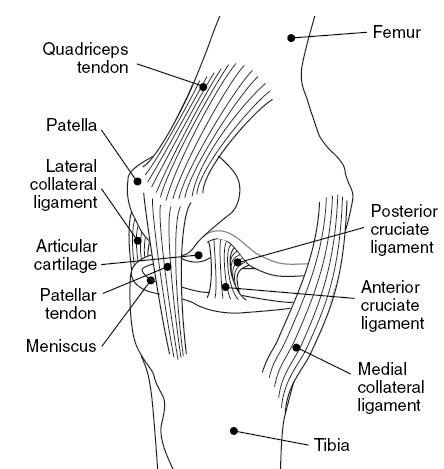
The knee joint is a complex hinge joint, made up of your thigh bone and shinbone, and kneecap which also joins to the thigh bone. To keep the knee stable we have four major ligaments. These are the:
These ligaments are responsible for providing stability to the knee and stopping it from collapsing. However if injured, the recovery time can be long term, ranging from 6 weeks for a minor sprain, up to around 12-14 months for a full rupture with surgical repair. Some evidence and studies are starting to display the potential for non operative ligament repair, however, these studies are in early stages and the long term impacts still are not fully understood.
As well as ligament injuries, there are other structures that are at risk within and around the knee, such as:
Different injuries to the knee have different risk factors.
ACL injury risk factors are arguably the most important to understand, as this ligament has the longest recovery time from knee injury. However, there have been many studies on the risk factors of ACL injuries, and the health science field is beginning to better understand how to minimise risk.
Some risk factors which been identified include:
Knee injuries can impact the lives of children, teenagers and adults. Whether you are physically active or not physically active at all, it’s likely at some point you will experience knee pain. Active people can have a tendency to do too much physical activity, and tip their body over the edge and risk injury. Inactive people generally don’t have a high enough level of strength and support around the knee, and can begin to experience pain when walking or getting out of a chair.
What’s interesting in Australia, is that studies have shown that the biggest increase in knee injuries over the last few years has been to the ACL. 5-14 year old girls have had one of the highest increases in ACL injury rate in Australia, and it continues to grow. However, it is not only in this age group where ACL injuries are becoming more prevalent, as it’s also growing within the general population. It’s important to seek professional advice on how to minimise the risk for this injury, as well as what to do if unfortunately it does occur.
Knee pain can be due to a variety of causes, and this increases the importance of having a professional diagnose the condition. As some knee injuries can take over 12 months to recover from, and can even be serious like infection, it would be best to have your injury looked at by a physiotherapist to get the correct diagnosis.
At Peak MSK Physio, our clinical team is trained in the examination, diagnosis and management of knee pain. We can help you better understand why your knee is hurting, and what you can do to feel like yourself again. In order to do so, this is where an accurate diagnosis is important. There are a variety of tests, imaging procedures and questions we can ask and utilise to gather YOUR diagnosis. With years of experience and training between the clinical team, you can trust them to help you and give you the right diagnosis and treatment of your knee injury.

There are various different methods to treat the knee. Options for manual therapy include:
As well as manual therapy, management will include exercise rehabilitation to make sure the knee is well supported. A focus on the quadriceps, hamstrings, glutes and core will likely play a major role in most knee rehab programs. Having good balance and symmetry in your movement will be a key focus of the rehab also, making sure the exercises are performed with the right technique to replicate how we want you to move.
Other aspects of management could include taping, ice and anti-inflammatory medication if deemed suitable for your specific injury. Your practitioner will advise you if referral to a specialist is required as part of your management plan.

Patello-femoral Pain Syndrome (PFPS) is a common condition that affects the front of the knee and can be a cause of ongoing knee pain, especially in athletes. It can cause pain during activities such as running, jumping, or walking up or down stairs. Physiotherapists are trained in the management of knee pain, and can assist with your treatment of PFPS, helping to alleviate pain and improve mobility.
PFPS is often caused by overuse or improper tracking of the patella (kneecap) as it moves over the femur (thigh bone). This can cause irritation and inflammation of the surrounding tissues, resulting in pain and discomfort. Physical therapy for PFPS typically begins with a thorough physical examination. The clinician will assess the patient's range of motion, strength, and overall function. Based on the assessment findings, a customised treatment plan will be developed.
One of the primary goals of physical therapy for PFPS is to reduce pain and inflammation. Your physiotherapist can do this by creating an exercise program specific to PFPS. Exercise has proven to be the most effective first line treatment for the condition. Your program will usually include exercises to target the quadriceps, hamstrings, and glutes, as well as the hip and core muscles. Strengthening these muscles can help to improve knee function and reduce the likelihood of further injury.
Additionally, manual therapy techniques such as massage, stretching, and joint mobilization may be used to help improve mobility at the patellofemoral joint. Taping att the knee can also be effective in the short term for pain relief. A physical therapist may also provide education on proper lower limb mechanics and activity modification. This can involve teaching patients how to perform exercises with proper form and technique, as well as strategies for avoiding aggravating activities.
PFPS can be helped by the guidance of a trained health professional. A skilled physical therapist can help to alleviate pain and improve mobility, as well as develop a comprehensive plan for preventing future injury. If you are experiencing knee pain or discomfort, book in to the clinic today so you can get your knee back on track.
In some cases you knee pain might go away on its own, but it’s likely to come back. Most instances of knee pain require a immediate course of action through a trained healthcare professional.
If your practitioner suspects a serious injury such as fracture, ligament damage or something more sinister like infection or cancer, you will be referred for other tests. This could be X-Rays, MRI’s or medication to name a few.
This will depend on your overall health, previous injury, and your metabolism to mention a few factors. From a physical perspective, strength, exercise levels and your body weight are important factors determining knee joint health.
At Peak MSK, we tailor programs specific to you and your health needs and what goals you have. We will do whatever we can to ensure we keep your knees and body healthy. Seek advice from our trained professionals to ensure you get the right advice, treatment and exercises.
Scientific evidence points to some knee conditions doing very well with an exercise approach, others do require surgery, then rehabilitation to recover. For example, the first line of help for an arthritic knee is exercise and you can check out our GLA:D programme here.
Our clinical team can provide you with an informed clinical opinion on the best advice and options for you to get back on the move.