A common presentation we see at Peak MSK here in Cheltenham is the patient with persistent buttock pain, with some referral down the back/side/front of the leg. Sometimes with pins/needles, tingles and sciatica like symptoms. The cause of these symptoms is something called deep gluteal syndrome (DGS), which will be discussed in more detail below.
What is Deep Gluteal Syndrome?
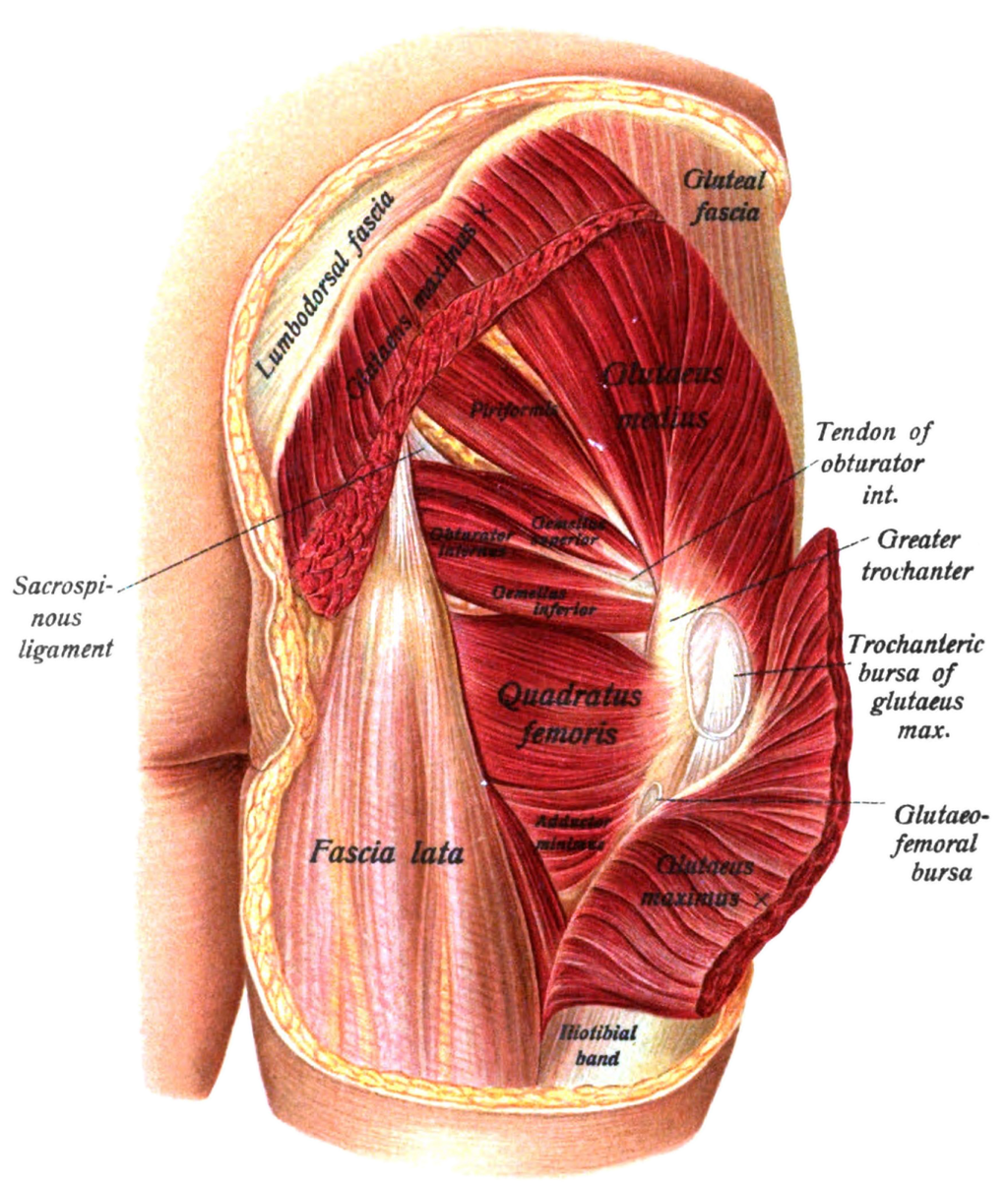
For many years, deep back side hip pain with radiating symptoms down the leg has been diagnosed as piriformis syndrome. The piriformis is a muscle that can be found on both sides of the body around the back of the hip. It runs from our tail (sacral) bone to the head of our thigh bone, the femur. It’s job is to mainly assist in rotation of the hip as well as stabilisation of our thigh bone.
The idea behind the diagnosis of piriformis syndrome was that the piriformis muscle was placing increased compression upon the sciatic nerve as it exited beneath, around or sometimes through the piriformis muscle. This was thought to occur with activities like increased sitting and weakness in the glutes, forcing the piriformis to work harder and further irritate the nerve.
Deep gluteal syndrome has been developed as an alternative diagnosis for piriformis syndrome. This is because other causes of sciatic nerve compression have been found to cause similar symptoms without involvement from the piriformis (1). Deep gluteal syndrome can be used as an umbrella term to cover the multiple forms of sciatic nerve compression. This can include:
- Compression from other muscles in the back of the hip. (Gemelli-obturator internus, quadratus femoris). The figure below illustrates the complex anatomy of this area.
- Formation of fibrous bands which compress the sciatic nerve.
- Narrowed space for the nerve to pass through.
- Certain hamstring conditions like tendon avulsions and injuries can cause inflammation and compression around the sciatic nerve.
What are the risk factors for Deep Gluteal Syndrome?
So now that you understand what deep gluteal syndrome is and what causes it, it is important to understand the risk factors for developing this injury. A major risk factor for developing deep gluteal syndrome is weak glutes (2). Upon examination of the glute complex, it is a common finding amongst patients suffering from deep gluteal pain to be weak through their glute muscles. The glutes, piriformis and those other smaller muscles above work together to create hip rotation, but when the glutes aren’t able to hold up their end of the partnership, the other muscles have to work harder, causing more strain and irritation around the muscle and the nerve. This can also cause the muscles to grow bigger and create less space for the nerve to operate.
A sedentary lifestyle with more sitting is another risk factor. Our glutes are less active when we are stationary for longer periods, and can again contribute to that weakness mentioned previously. More sitting means that not only are the glutes less active, but that constant compression is being placed between the sciatic nerve and the muscular and fibrous structures in the back of the hip. This commonly exacerbates symptoms in those suffering from deep gluteal syndrome and should be kept to low levels if possible.
How is Deep Gluteal Syndrome diagnosed?

Diagnosis of deep gluteal syndrome can be performed by a physiotherapist. They have a set of clinical tests they can use which will reproduce one's symptoms and indicate positive DGS signs (2)(3).
A skilled clinician will also ask about lifestyle. As mentioned previously, being more sedentary can contribute to the presence of deep gluteal syndrome. Understanding if somebody has been sitting more than usual is a key factor relating to this condition.
Strength testing and manual muscle testing of the lower limb is also a key part of the physical assessment. This can be assessed with technology such as a dynamometer or muscle metre. We possess both at Peak MSK and it helps us gather accurate strength data in our testing. With DGS, the focus would be on the glutes and comparing the strength/endurance/power of the affected side.
What is the management for Deep Gluteal Syndrome?
Management for DGS should always first consist of education on the injury and conservative measures like exercise and manual therapy for at least six weeks (2). Soft tissue treatment to the muscles impacting on the sciatic nerve can help provide pain relief, as well as manual treatment to the low back joints and the hip to improve mobility if that has been limited due to injury. Manual therapy will provide relief, but it will likely only be short lived, which is why the exercise component of treatment is so important.

Exercise rehabilitation in the early stages should consist of stretching to the hip, low back and nerve. There are a variety of different ways that this can be done, which is why they should be delivered by one of our Physiotherapists. Too much of the wrong stretching could further exacerbate symptoms and only make problems worse. Nerves are sensitive structures and need precisely the right amount of exercise and movement to improve.
There are some rare instances where conservative treatment does fail and that can lead to a few different options. Non-steroidal anti-inflammatory drugs (NSAIDs) administered from the GP can be an option if other conservative measures fail. If there is inflammation around the nerve, settling this down can provide some relief and help the exercises become more effective.
If a combination of NSAIDs and exercise still don’t provide enough relief, then more invasive measures could be required. Imaging will likely be needed to confirm the exact cause of sciatic nerve entrapment (3). Once the exact cause of entrapment is identified, a review with a sports physician or orthopaedic surgeon will likely be needed to determine if surgery is required. Corticosteroid injections have been found to be beneficial before undergoing surgery, but symptoms can return and it isn’t always successful. Surgery is quite a complex procedure but generally involves decompressing the sciatic nerve by altering or removing part of the problem structure (3).
If surgery or referral is required, post-operative rehabilitation by a trained health professional is recommended for a better and quicker recovery. The clinical team at Peak MSK can help you with those next steps if required.
Most importantly, Train The Glutes!
As mentioned earlier, glute training will be an essential part of management so we can offload those other muscles a bit more (4). It’s important to know we have 3 different glute muscles, and each plays slightly different roles in our everyday movement.

Firstly, let's start with the big one, our glute max. Our glute max muscle runs from the middle of our pelvis and fans around to the outside of our thigh bone. It helps rotate and swing our hip outwards as well as push our hip backwards. A simple and easy way to train the glute max muscle is with glute bridges. This primarily trains that backwards hip motion and with the addition of a band, you can add in that rotation component also.
Next, we have our glute medius. This muscle runs from the top of our hip bone and attaches at the outer part of our thigh bone, similarly to our glute max. It also, much like our glute max, helps swing the hip away from the body but rather than rotate outwards, the glute medius helps rotate the hip inwards. It also plays a role in the stabilisation of our pelvis. Crab walks are a great way to train the gluteus medius muscle.
Finally, we have our gluteus minimus. The smallest of the glute muscles, it runs a similar path to the glute med starting at the hip bone and finishing on the outside of our thigh bone. It basically does the same action as our glute med muscle in that it helps rotate the hip inwards and swing the hip outwards. You can target gluteus minimus with exercises that target the gluteus medius also, so crab walks will help build this muscle up too.
Now You Know!
So hopefully now you have a better understanding about what is causing that deep pain around the back of the hip and down into the leg. With the right management, you can get on top of the condition early and be back doing the activities you love in no time.
Remember, you need to rule in and rule out whether it is the back or the hip causing this issue. From there, your management needs to be targeted towards alleviating the nerve compression. Stretching, hands on treatment and exercises can help with this. Medication might be needed in some cases where pain and inflammation are high. This will of course require your GP to be involved in treatment. If all conservative measures fail, then there is the potential for other treatments like injections and surgery, but only in very extreme cases are these indicated.
DGS isn’t something that will just go away, and it will require about 6 weeks of management, so it’s best if you get onto it sooner rather than later. If you feel like deep gluteal syndrome could be the cause of your pain, call up our clinic today and schedule an appointment with one of our trained clinicians who can diagnose and manage it for you.
Section: FAQ
Do I need an X-Ray or MRI to diagnose this injury?
In most cases imaging will not be necessary for the management and diagnosis of DGS. If required, imaging can be utilised further down the track to confirm what is causing sciatic nerve compression.
Can I suffer nerve damage from this injury?
In most cases, DGS will recover within 6 weeks of management. If left untreated, there is the potential to be longer lasting effects.
Will Medication help?
Medication will potentially be a part of management to control inflammation or pain if it is severe. This will likely require us to get your GP involved in management if they are not already.
Should I Ice? Heat? Rest?
Heat can be useful as will rest in severe cases. Your clinician will provide you with the best acute form of management. Read about PEACE and LOVE here.
Could it be coming from my back and hip?
Yes, there is the potential for both structures to be causing irritation of the sciatic nerve.
Should I see the physio or self-manage?
Physiotherapists are skilled in the recognition and management of DGS. This allows optimal recovery to your sports season needs as well as prevention advice and screening for other issues. Rest assured we will give you a self-management strategy, that is much better than looking on the web.
Can DGS go away on its own?
Unless you target the structure causing the compression, it is unlikely that DGS will just go away. Some people leave the injury for months only for it to get gradually worse over time.